Jawbone cavitations, particularly following wisdom tooth extractions, are increasingly being studied for their potential to harbor infections and trigger systemic health issues. This problem can arise when the periodontal ligament—the connective tissue that holds the tooth in place—is not completely removed during extraction, leaving behind a space where bacteria can thrive. This leads to what is known as cavitational osteonecrosis or jawbone cavitation.
Mechanisms of Jawbone Cavitation
1. Periodontal Ligament Left Behind: After wisdom tooth extraction, if the periodontal ligament is not completely removed, the healing process may be impaired. The ligament can trap bacteria in the area, and the body may fail to fill the space with healthy bone tissue. Instead, this area becomes a breeding ground for bacteria, toxins, and even necrotic (dead) tissue, leading to a chronic low-grade infection that can spread throughout the body via the bloodstream and lymphatic system.
2. Chronic Inflammation: The bacteria and toxins released from a jawbone cavitation can cause chronic inflammation, similar to the mechanism seen with infected root canals. The immune system is continuously stimulated in an effort to clear the infection, but the isolated nature of the cavitation makes it difficult for the body to effectively target and eliminate the bacteria. This chronic inflammatory state has systemic effects, contributing to conditions like brain fog, fatigue, and autoimmune dysfunctions.
3. Biofilm Formation: Cavitations, like root canals, can become filled with bacterial biofilms, which are communities of bacteria that are resistant to the immune response and antibiotic treatment. These biofilms act as a reservoir for ongoing infection, leading to persistent inflammation and potential health problems in other parts of the body.
Links to Systemic Health Problems
1. Neurological Illness: Bacteria and their toxins from a jawbone infection can enter the bloodstream and trigger neuroinflammation. This chronic inflammation in the brain has been associated with neurological conditions such as Parkinson’s disease, multiple sclerosis (MS), and ALS. Inflammatory cytokines produced in response to the infection can cross the blood-brain barrier, leading to cognitive issues such as brain fog and contributing to neurodegenerative processes.
2. Cancer: While direct links between cavitations and cancer are still being researched, the chronic inflammation and immune dysregulation caused by ongoing bacterial infections are known to be risk factors for cancer development. Chronic infection can promote the release of proinflammatory cytokines and oxidative stress, both of which are factors in cancer progression.
3. Fatigue and Lyme Disease: Persistent jawbone infections can drain the body’s resources and lead to chronic fatigue, as the immune system is constantly fighting the infection. Moreover, patients with conditions like Lyme disease are particularly vulnerable to jawbone cavitations, as their immune systems are already compromised. The toxins from cavitations may worsen Lymerelated symptoms, exacerbating issues like fatigue, brain fog, and joint pain.
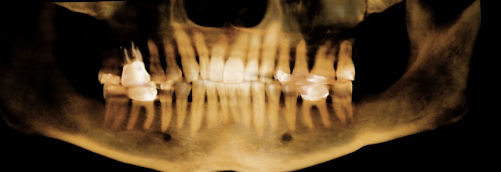
Diagnostic Challenges: 2D Imaging vs. Cone Beam 3D CT
• Limitations of 2D Imaging: Standard two-dimensional dental X-rays are inadequate for diagnosing cavitations and other hidden infections. 2D images provide only a flat view, making it difficult to detect subtle bone loss or small pockets of infection in the complex threedimensional structure of the jaw. Many cavitations remain undetected on traditional X-rays due to their limited resolution and depth.
• Importance of Cone Beam 3D CT: A cone beam CT (CBCT) scan offers a three-dimensional view of the jaw and surrounding structures, making it the gold standard for detecting cavitations. This technology can reveal hidden bone loss, infections, and areas where necrotic tissue has developed that would otherwise go unnoticed. It also allows for the visualization of fine structures in the jawbone, providing a far more detailed and accurate diagnosis of cavitations.
Treatments for Jawbone Cavitations
Several treatments have been proposed for dealing with jawbone cavitations, with biological dentistry focusing on approaches that target the infection while supporting the body’s natural healing processes.
1. Ozone Therapy: Ozone is a powerful oxidizing agent that can be injected into the cavitation site to kill bacteria, viruses, fungi, and other pathogens. It works by oxidizing the cell walls of bacteria, leading to their destruction. Ozone also promotes oxygenation and healing in the affected tissues. After ozone therapy, the cavitation site is cleaned, removing dead tissue and bacteria, promoting better healing.
2. Platelet-Rich Fibrin (PRF) or Platelet Plug: After the infection has been treated, some biological dentists use a platelet plug, derived from the patient’s own blood, to help seal the cavitation and encourage bone regeneration. This technique involves drawing the patient’s blood, processing it to concentrate the platelets, and then injecting the platelet-rich plasma (PRP) or platelet-rich fibrin (PRF) into the cavitation site. Platelets contain growth factors that stimulate tissue healing and regeneration, helping the jawbone heal more effectively.
3. Surgical Debridement: In cases where ozone therapy and PRF are insufficient, surgical debridement of the cavitation may be necessary. This involves removing any necrotic bone or infected tissue to prevent the spread of the infection and allow healthy bone to grow in its place.
4. Post-Treatment Support: After treatment, patients often benefit from immune support through supplements like vitamin D, vitamin C, and probiotics to help the body recover from the chronic infection. Detoxification protocols, such as lymphatic drainage or chelation therapy, may also be recommended to support the body’s ability to clear toxins from the infection site.
Literature on Jawbone Cavitations and Systemic Disease
• Studies have shown a connection between chronic oral infections and systemic diseases, including neurological conditions, autoimmune disorders, and cardiovascular diseases. A paper by Bouquot and others emphasized the prevalence of ischemic osteonecrosis (cavitations) and their potential role in systemic diseases.
• The role of oral infections in neurodegenerative diseases is also gaining attention, with researchers examining how chronic inflammation from sites like root canals and cavitations may trigger neuroinflammation and increase the risk of conditions like Alzheimer’s disease, MS, and Parkinson’s disease.
Conclusion
Jawbone cavitations are an often-overlooked source of chronic infection that can have significant systemic effects. From neurological conditions to fatigue and autoimmune disorders, the persistent presence of bacteria and inflammation in the jaw can contribute to a wide range of health problems. Accurate diagnosis using cone beam 3D CT imaging and effective treatments like ozone therapy and platelet plugs can help address these infections and promote healing.
For those looking for further insights, in our podcast below, we discuss how chronic inflammation triggered by infected root canals could potentially exacerbate conditions like MCAS. Watch it to learn more: