Lyme has been an identifiable disease for over 40 years. When people hear ‘Lyme disease,’ they usually think of bacteria, particularly Lyme Borrelia. The media and public health officials pay attention to ticks and Lyme disease exposure and risk. Treatment information is on eradicating Lyme bacteria. The focus is predominately on acute Lyme and what to do for prevention after a tick bite. This is all good stuff, but not representative of the actual Lyme disease epidemic.
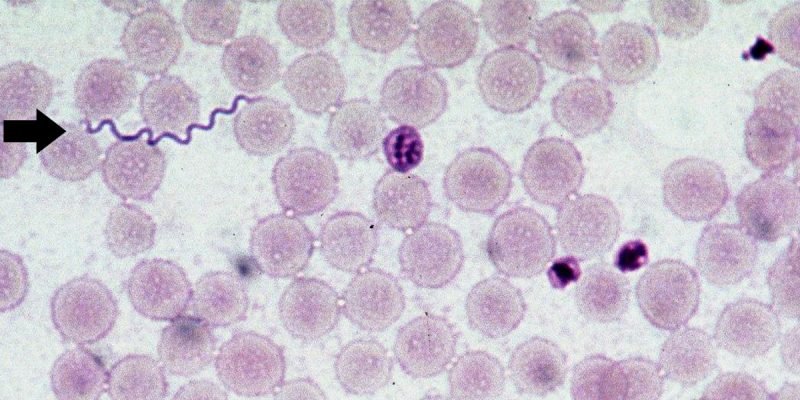
Lyme is the front disease for a myriad of infections. Logically, does a tick carry one bacterial infection? Highly unlikely. Ticks are like dirty needles carrying multiple infections in the form of bacteria, viruses, and parasites. An infected person gets as many as 5-10 infections. In addition, when the immune system is compromised or dysfunctional from battling Lyme infection, additional opportunistic infections that are dormant in the body become activated.
So, focusing on just Lyme bacteria for diagnosis and treatment limits recovery. Unfortunately, many coinfections (as they are referred to) are challenging to test for and diagnose. Symptoms are overlapping. The probability of having coinfections, however, is exceptionally high. It has been generally estimated through clinical experience to be about 80%, but a recent survey in 2016 in the U.K. reported that 94% of Lyme disease patients have at least one coinfection. Here is a summary of the common coinfections.
Bartonella infects red blood cells and the cells that line blood vessels. Common symptoms are neurological, persistent headaches, chronic fatigue and muscle pain, and pain in the soles of the feet. Other symptoms are severe insomnia, migraines, anxiety, constant worry, agitated depression, panic attacks, psychosis, bipolar disorder, depression, agitation, autistic-like symptoms, hallucinations, memory loss, brain fog, and aggression, sometimes referred to as “Bartonella rage”. A person may only have just one symptom or many of them. Bartonella has been documented in patients with rheumatoid arthritis (RA), fibromyalgia, and multiple sclerosis (MS).
Babesia is a malaria-like parasite that infects red blood cells. Classic babesia symptoms include drenching sweats anytime during the day and frequently at night. Thermal dysregulation can go from feeling cold to chills to drenching sweat in minutes. Headaches often in the front and sometimes in the back of your head, or your head feels like it is in a vice grip. Mood instability, insomnia, depression, anxiety, balance problems, or tinnitus that change all the time and are caused by inflammation of the brain and meninges. Heart palpitations or any cardiac irregularity (pulse, blood pressure). Air hunger (gasping for a breath). Severe babesia can mimic cancer.
Mycoplasma are the smallest of all bacteria. They can change their shape and fit into areas other bacteria cannot. It commonly infects the synovial lining of joints. Fatigue is a common symptom. Because it scavenges fats from the myelin sheath covering nerve tissue, mycoplasma is linked to RA, MS, ALS, and Parkinson’s. Mycoplasma has been found in 75% of Lyme patients, 90% of RA patients, and 80% of Chronic Fatigue and Fibromyalgia patients.
Ehrlichiosis is a term that describes several different bacterial diseases, one of which is anaplasmosis. The clinical presentations of ehrlichiosis and anaplasmosis are the same. Symptoms include sudden high fever, fatigue, muscle aches, and headache. The disease can be mild or life-threatening. Severely ill patients can have low white blood cell count, low platelet count, anemia, elevated liver enzymes, kidney failure, and respiratory insufficiency. Ehrlichiosis/anaplasmosis is often suspected in a patient who does not respond well to treatment for Lyme disease.
Coxsackie viruses are tiny viruses in the intestines and the stool. There are two main groups: type A and type B, each with smaller groups of different strains of coxsackie viruses. Symptoms are fever, sore throat, diarrhea, vomiting, rash, muscle pains, liver inflammation, and inflammation of the heart sack. Coxsackie virus is the agent that causes hand, foot, and mouth disease. The virus can cause Bornoholm disease, an infection of the pleura (pleuritis) that results in severe chest pains.
Chlamydia pneumoniae (CPN) is an intercellular bacteria that hijacks the energy of its human hosts by stealing power from the cells to grow (ATP). This often results in extreme exhaustion, but symptoms include burning pains in the chest, the bones, or the muscles. It usually infects lung tissue but can spread to the connective tissues, nerve tissues, brain, and muscles. It infects cells in veins and the lymphatic system. Symptoms are broad and include pneumonia, meningoencephalitis, arthritis, myocarditis, connective tissue pains (fibromyalgia), asthma, infections of the airways, bronchitis, MS-like complaints, Gillian Barre, Alzheimer’s, atherosclerosis, and shortness of breath.
Epstein Barr Virus (EBV) is a viral illness in the same family as herpes and chickenpox. EBV infects 95 percent of humans, but it is usually dormant in the body and rarely reactivates, usually only in times of stress. Chronic EBV infection is something that is only seen in people with immune problems, such as Lyme disease, transplant patients, HIV patients, or people born missing a part of their immune system or immune function. Dormant viruses like EBV can be activated in the presence of Lyme disease. This can accelerate debilitating fatigue as well as many other autoimmune and neurological symptoms. Research repeatedly shows abnormal accumulations of EBV in MS patient’s brain lesions. Patients suffering from other autoimmune diseases had similar findings regarding their pathological tissues.
Cytomegalovirus (CMV) is a member of the herpes family and shares the standard ability to remain alive, yet dormant, in the human body for the life of its human host. About 80 percent of adults are infected with the disease. CMV, however, rarely becomes active unless the immune system is weakened and cannot hold the virus in check. Trauma or decreased immune system function in conditions such as Lyme disease can awaken CMV. Symptoms include prolonged high fever, chills, severe fatigue, swollen lymph glands, headache, and an enlarged spleen. People with weakened immune systems are at risk for more severe complications, including pneumonia, liver infection, and anemia.
Parasites are considered the most significant opportunistic infection. Not limited to the intestines (gut), parasites inhabit many other body parts, including the brain. Many parasites take control of their hosts’ minds. With Lyme disease, parasites limit a person’s drive and motivation to get well. They become convinced they are not sick and that aggressive treatment is not required. Treating parasites can unlock unprecedented improvement in body-wide symptoms like brain fog, depression, irritability, memory loss, anxiety, and fatigue. A significant finding is that many other infections hide inside parasites for protection. For example, Lyme’s Borrelia bacteria hides inside parasitic worms, causing chronic brain diseases. As a result, if parasites are untreated, progress against other infections, like Borrelia, Babesia, and Bartonella, can be impaired or halted.
A fascinating occurrence is that these coinfections want to be the lead infection and present their symptoms first and foremost, actually pushing Lyme symptoms into the background. The symptoms that a person suffering from Lyme disease reports are often the symptoms of coinfections.
Treating coinfections can result in a dramatic reduction of symptoms, and people feel like they have beaten their Lyme disease. The Lyme infection is likely still present and must be addressed with comprehensive treatment.
While treatment directed at the Lyme bacteria is essential, so are treatments targeted at the coinfections, especially viruses and parasites. Since most patients present with chronic Lyme that has been undiagnosed or untreated for months, years, or decades, lots of time has passed for these infections to take hold in the body. This is one of the primary reasons why recovery from Lyme disease is so difficult. You are not battling one bacteria; you are actually fighting multiple infections that invade many different parts of the body.