Infected root canals can indeed lead to significant immune system dysregulation and trigger conditions like mast cell activation syndrome (MCAS). This happens through a combination of chronic infection, inflammation, and the body’s complex immune responses to the persistent presence of harmful bacteria
or toxins.
Mechanisms by Which an Infected Root Canal Affects the Immune System
1. Chronic Low-Grade Infection
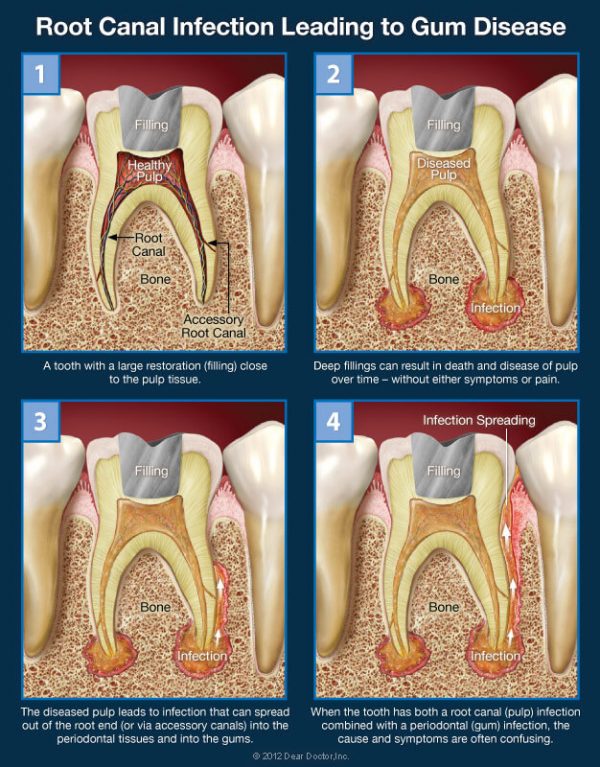
When a root canal becomes infected, bacteria can inhabit the intricate network of tiny tubules and spaces inside the tooth, making complete sterilization challenging. These bacteria may produce toxins and other inflammatory by-products that leak into surrounding tissues. The immune system continuously tries to fight off this infection, leading to chronic low-grade inflammation that affects the body systemically.
2. Immune Dysregulation
The immune system can become overwhelmed when exposed to persistent, low-level bacterial toxins from an infected root canal. This may lead to immune dysregulation, wherein the immune system begins to either overreact to benign stimuli or fails to adequately regulate inflammatory responses. This is where conditions like Mast Cell Activation Syndrome (MCAS) come into play. In MCAS, mast cells release excessive amounts of inflammatory mediators (like histamine) in response to triggers, potentially initiated by the ongoing bacterial toxins from the infected root canal.
3. Toxic By-products and Cytokine Storms
Infected root canals often harbor anaerobic bacteria that produce potent endotoxins and exotoxins. These toxins can enter the bloodstream, leading to systemic effects. The immune system responds by releasing cytokines, signaling proteins that control immune responses. An excessive release of cytokines can lead to what is called a cytokine storm, an overreaction of the immune system that results in widespread inflammation and tissue damage.
4. Oral-Systemic Link
The health of the mouth is closely linked to overall systemic health. An infection in the mouth can spread via blood vessels or lymphatic systems, causing inflammation and infection in distant parts of the body. Studies have shown correlations between oral infections and systemic diseases like cardiovascular disease, autoimmune disorders, and chronic inflammatory conditions. For people prone to immune system imbalance, an infected root canal can act as a persistent irritant that triggers widespread immune activation.
5. Biofilms
Root canals are particularly prone to biofilm formation, where bacteria cluster together in protective communities that are more resistant to the body’s immune response and antibiotic treatments. These biofilms can become a reservoir of chronic infection, continually stimulating the immune system without being eradicated, which may perpetuate dysregulation.
Link to Mast Cell Activation Syndrome (MCAS)
Mast cells are part of the immune system and are typically involved in allergic responses and tissue repair. In MCAS, mast cells become dysregulated and start releasing excessive amounts of histamine, cytokines, and other inflammatory mediators. This can result in symptoms like hives, digestive issues, brain fog, and cardiovascular symptoms.
An ongoing infection in the root canal can continually activate the immune system and mast cells, keeping the body in a heightened state of inflammation. For susceptible individuals, this might be enough to trigger or worsen MCAS, as the immune system is constantly on high alert due to the presence of toxins or bacteria from the root canal infection.
For those looking for further insights, in our podcast below, we discuss how chronic inflammation triggered by infected root canals could potentially exacerbate conditions like MCAS. Watch it to learn more:
Limitations of Standard X-Rays in Detecting Infected Root Canals
A standard 2D dental X-ray, while useful for many dental diagnostics, often fails to capture the full extent of an infection in a root canal. This is due to several factors:
• 2D View: Standard X-rays provide only a two-dimensional view, which can make it difficult to see infections or abscesses that are present in the complex, three-dimensional structure of a tooth, particularly the root tips or areas around the surrounding bone.
• Obscured Infections: An infection might be obscured by dense bone or structures overlapping the infected area in the X-ray view. Since X-rays flatten the image, small or hidden infections can easily be missed.
• Early Infections: Infections that are just starting to form might not yet have caused enough bone loss or tissue changes to be visible on an X-ray. It is typically the bone resorption (loss) around the tooth root, caused by the infection, that appears on the X-ray, not the infection itself.
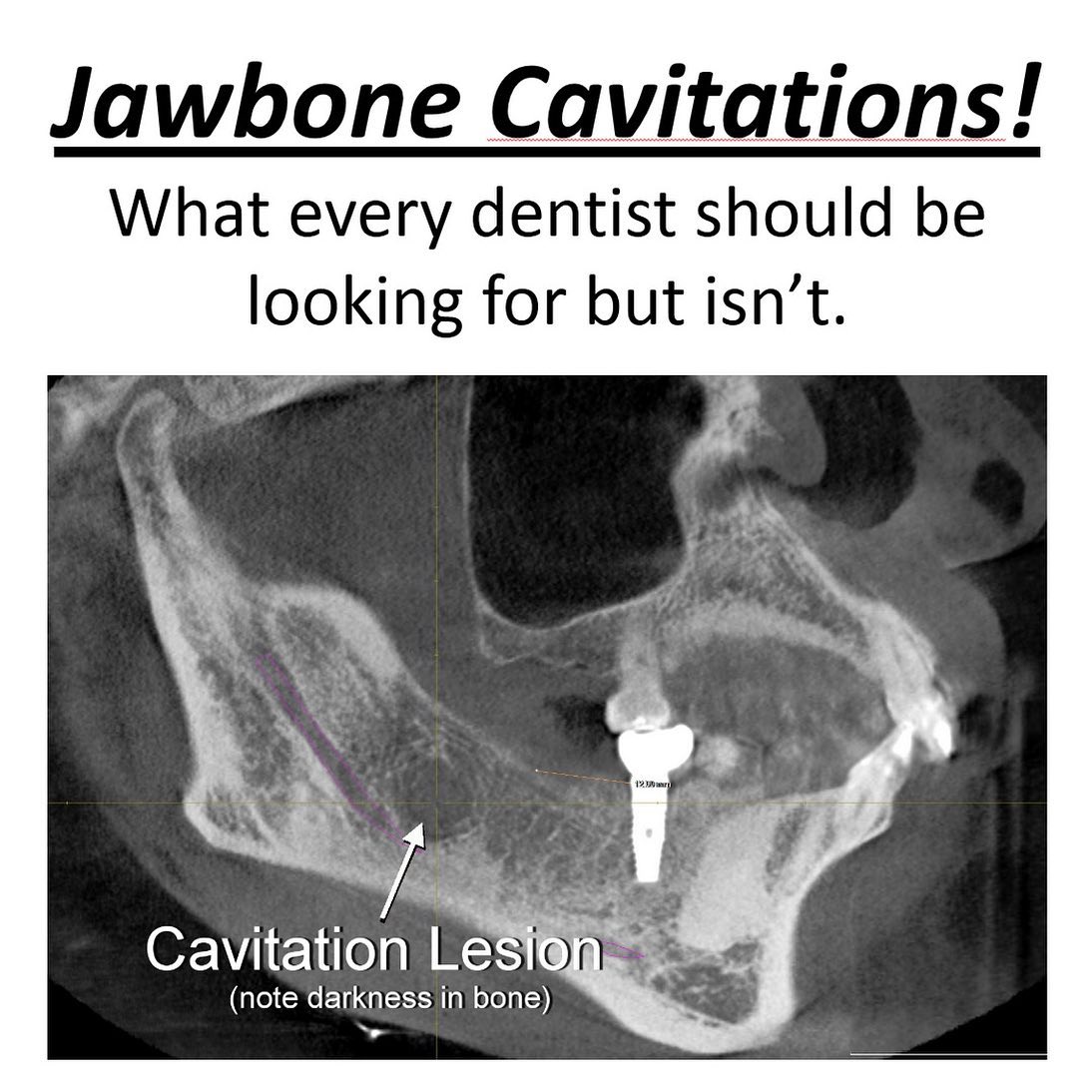
Importance of a 3D Cone Beam CT Scan
The limitations of standard X-rays make a 3D cone beam CT (CBCT) scan the gold standard for diagnosing root canal infections that might otherwise go undetected.
• 3D Visualization: A CBCT provides a three-dimensional view of the entire tooth and surrounding structures. This enables a far more detailed and accurate assessment of the root canal and its surrounding tissues, detecting infections that might be invisible on 2D X-rays.
• Better Detection of Bone Loss: The CBCT can detect even small amounts of bone loss or subtle changes in the periapical region (the area around the tooth root), which might be early signs of infection.
• Hidden Canals and Fractures: Root canals often have multiple canals, and some can be extremely small or hidden. A CBCT can reveal these extra canals and diagnose vertical fractures or periapical cysts, which are often missed on traditional X-rays.
• Accurate Diagnosis of Abscesses and Granulomas: CBCT scans are highly sensitive to detecting periapical abscesses (pus-filled infections) and granulomas (chronic inflammatory lesions), both of which may go unnoticed on standard X-rays.
Conclusion
Infected root canals are more than just a localized dental issue; they can have systemic repercussions by triggering immune system dysregulation, chronic inflammation, and conditions like mast cell activation syndrome. Standard X-rays are often insufficient to detect the full extent of root canal infections due to their two-dimensional nature, leading to missed diagnoses. A 3D cone beam CT scan offers a far more detailed and accurate assessment, enabling the detection of hidden infections, bone loss, abscesses, and other dental pathologies that can contribute to systemic health issues.